Role of PCR Machines in Disease Detection
Strategic Role of PCR in Modern Diagnostics
Polymerase Chain Reaction (PCR) machines have fundamentally reshaped modern disease detection by enabling laboratories to identify pathogens at the molecular level with remarkable accuracy. Unlike traditional diagnostic tools that rely on visible symptoms or slow-growing cultures, PCR works by detecting the genetic material of viruses, bacteria, and other microorganisms. This precision allows clinicians to confirm infections earlier and make informed treatment decisions faster. In today’s healthcare environment, where rapid response and diagnostic certainty matter, PCR machines serve as a critical backbone of hospital labs, research centers, and public health surveillance systems worldwide.
Molecular Principles of PCR Technology
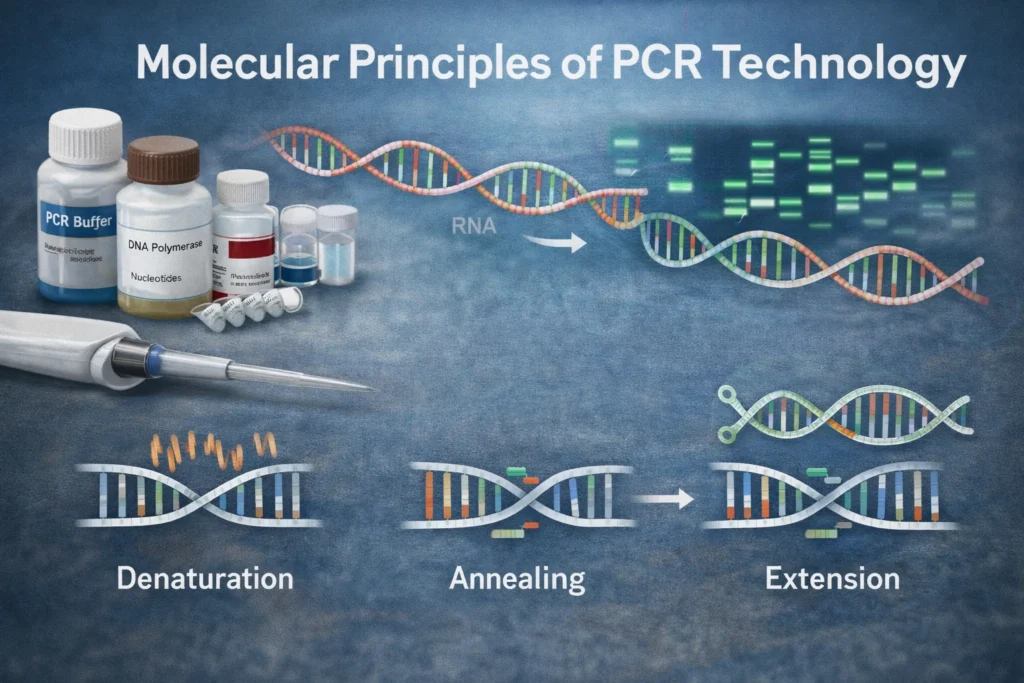
At its core, PCR technology is built on the principle of amplifying specific segments of DNA or RNA to detectable levels. Even if only a tiny amount of genetic material is present in a sample, PCR can replicate it millions of times within hours. This amplification makes previously invisible pathogens measurable and clinically relevant. The process depends on temperature cycling, specialized enzymes, and short DNA sequences called primers that target unique regions of a pathogen’s genome. By focusing only on specific genetic signatures, PCR ensures highly selective and reliable disease identification.
You Might also Like: Leonaarei Explained: Meaning, SEO & Future Impact
Core Components of PCR Systems
A PCR system is more than just a machine it is a coordinated molecular environment designed for precise replication. The central instrument, known as a thermocycler, controls rapid temperature shifts required for amplification. Essential reagents include DNA polymerase enzymes, primers, nucleotides, and buffer solutions that maintain optimal chemical conditions. Modern systems often integrate fluorescence detection modules for real-time analysis. Together, these components create a controlled reaction chamber where genetic material can be copied accurately, consistently, and at high speed, ensuring dependable diagnostic performance across clinical settings.
Mechanism of DNA and RNA Amplification
PCR amplification follows a repeating cycle that selectively multiplies target genetic material. Through controlled heating and cooling phases, DNA strands separate, primers attach to specific sequences, and polymerase enzymes synthesize new strands. For RNA viruses, an additional reverse transcription step converts RNA into complementary DNA before amplification begins. This cyclical process exponentially increases the number of copies, allowing detection even when pathogen levels are extremely low. The efficiency of this mechanism is what makes PCR one of the most sensitive molecular diagnostic technologies available today.
Thermocycling Phases Explained
Each PCR cycle includes three primary stages: denaturation, annealing, and extension. During denaturation, heat separates the DNA strands. In the annealing phase, primers bind to their target sequences. Finally, extension allows polymerase enzymes to build new DNA strands. These steps repeat multiple times, doubling the genetic material with each cycle and creating millions of precise copies within a short timeframe.
Clinical Types of PCR Techniques
Over time, PCR technology has evolved into multiple specialized formats tailored for clinical diagnostics. Conventional PCR detects amplified DNA at the end of the reaction, while real-time PCR (qPCR) monitors amplification as it happens, offering quantitative insights. Reverse transcription PCR (RT-PCR) is specifically used for RNA viruses, converting RNA into DNA before amplification. Digital PCR further enhances sensitivity by partitioning samples into thousands of micro-reactions. Each variation expands the clinical utility of PCR, enabling accurate detection across infectious diseases, oncology, genetics, and beyond.
PCR in Infectious Disease Surveillance
PCR machines play a central role in infectious disease surveillance by enabling early and accurate pathogen identification. Public health laboratories rely on PCR platforms to monitor outbreaks, detect emerging strains, and track transmission patterns within communities. Because PCR identifies infections based on genetic material rather than symptoms alone, it can detect cases before they become clinically obvious. This early insight helps healthcare authorities implement containment strategies, reduce spread, and allocate medical resources effectively. In both hospital and community settings, PCR serves as a frontline tool for proactive disease monitoring.
Viral Pathogen Detection Using PCR
Viral infections often present diagnostic challenges due to overlapping symptoms and low early viral loads. PCR machines address this challenge by targeting unique viral genetic sequences, allowing precise identification even in the earliest stages of infection. From respiratory viruses to bloodborne pathogens, PCR-based assays provide rapid confirmation that supports timely treatment decisions. The ability to detect RNA viruses through reverse transcription PCR has been particularly transformative. By identifying viral presence before antibody development, PCR reduces diagnostic delays and improves patient outcomes in acute and high-risk cases.
Bacterial and Parasitic Identification via PCR
Traditional bacterial culture methods can take days to deliver results, and some pathogens are difficult to grow in laboratory conditions. PCR eliminates this limitation by detecting bacterial and parasitic DNA directly from clinical samples. This capability significantly shortens diagnostic timelines and improves detection accuracy. In cases of bloodstream infections, sexually transmitted infections, or gastrointestinal diseases, PCR provides reliable confirmation when speed is critical. The molecular precision of PCR also allows differentiation between closely related strains, helping clinicians choose targeted antimicrobial therapies with greater confidence.
PCR in Pandemic and Outbreak Response
During global health emergencies, rapid and scalable testing becomes essential. PCR machines have consistently demonstrated their value in pandemic response by delivering high-throughput, accurate diagnostics. Large laboratory networks can process thousands of samples daily using automated PCR systems. This scalability supports mass testing, early case identification, and isolation protocols. Beyond diagnosis, PCR also contributes to epidemiological research by identifying genetic variations in pathogens. In outbreak scenarios, reliable molecular detection strengthens public health strategies and enhances preparedness for future infectious threats.
Advantages of PCR Over Conventional Diagnostics
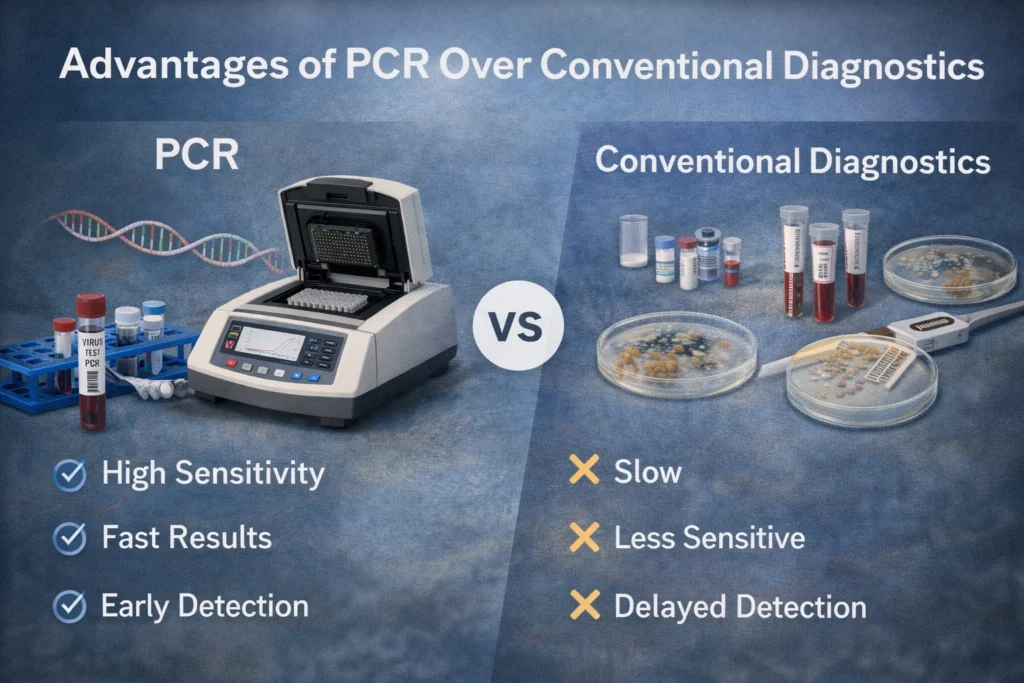
Compared to conventional diagnostic methods, PCR offers superior sensitivity, specificity, and turnaround time. While culture-based testing depends on microbial growth and serological assays rely on immune response, PCR directly detects pathogen genetic material. This means infections can be identified even when organisms are present in very low concentrations. Additionally, PCR minimizes false negatives in early-stage infections. Its ability to deliver accurate results within hours instead of days improves clinical decision-making, reduces unnecessary treatments, and supports more efficient healthcare delivery across diverse medical environments.
You Might also Like: Kompama: The Innovative Concept Redefining Digital Authority
PCR vs Serological Testing
Serological tests detect antibodies produced by the immune system, which may take days or weeks to appear after infection. PCR, in contrast, identifies the pathogen’s genetic material directly, allowing much earlier diagnosis. While serology helps assess past exposure, PCR is more effective for confirming active infections. This distinction is critical in acute care and outbreak control settings.
Diagnostic Precision of Real-Time PCR (qPCR)
Real-time PCR, commonly known as qPCR, enhances traditional PCR by measuring amplification as it occurs. Using fluorescent markers, qPCR provides quantitative data on pathogen load, offering deeper clinical insights beyond simple detection. This real-time monitoring improves accuracy and reduces contamination risk since results are analyzed within a closed system. In infectious disease management, viral load measurement helps assess disease severity and monitor treatment response. The precision and speed of qPCR make it one of the most widely adopted molecular diagnostic tools in modern laboratories.
Advanced PCR: Multiplex and Digital Platforms
As diagnostic needs grow more complex, advanced PCR platforms have expanded the capabilities of traditional systems. Multiplex PCR allows simultaneous detection of multiple pathogens within a single reaction by using different primer sets. This approach improves efficiency and reduces testing time, especially in respiratory or gastrointestinal panels. Digital PCR takes precision even further by dividing samples into thousands of micro-reactions, enabling absolute quantification without standard curves. These innovations enhance diagnostic accuracy, improve laboratory throughput, and support high-demand clinical environments where speed and reliability are equally important.
Limitations and Technical Challenges of PCR
Despite its strengths, PCR technology is not without challenges. Contamination risks can lead to false positives if laboratory protocols are not strictly followed. Additionally, PCR requires specialized equipment, controlled environments, and trained personnel. In low-resource settings, cost and infrastructure limitations may restrict accessibility. Another consideration is the possibility of detecting non-viable genetic fragments, which may not represent active infection. Understanding these limitations ensures that clinicians interpret PCR results appropriately and combine them with clinical evaluation for comprehensive patient assessment.
Sensitivity and Limit of Detection
Sensitivity refers to a test’s ability to detect even minimal amounts of genetic material. The limit of detection (LoD) defines the smallest concentration of a pathogen that can be reliably identified. While high sensitivity is a major strength of PCR, extremely low detection thresholds may sometimes identify residual or clinically insignificant fragments. Laboratories must carefully validate assays to balance sensitivity with clinical relevance.
Quality Control in PCR Laboratories
Maintaining accuracy in PCR diagnostics depends heavily on rigorous quality control measures. Laboratories implement standardized workflows, calibration protocols, and contamination prevention strategies to ensure reliable results. Internal controls are included in each run to confirm proper amplification, while external validation verifies assay performance over time. Accreditation standards and regulatory guidelines further strengthen laboratory accountability. Consistent documentation, technician training, and equipment maintenance all contribute to dependable outcomes. Strong quality assurance practices transform PCR from a powerful technology into a trusted diagnostic solution across healthcare systems.
Future Directions of PCR in Precision Medicine
The future of PCR technology is closely linked to the evolution of precision medicine. Portable and point-of-care PCR devices are becoming more compact, enabling rapid testing in clinics, emergency settings, and even remote locations. Integration with digital health systems and data analytics platforms will enhance real-time disease tracking and personalized treatment decisions. Advances in automation and microfluidics are expected to reduce processing times while increasing scalability. As molecular diagnostics continue to evolve, PCR machines will remain central to targeted therapies and individualized patient care.
Point-of-Care PCR Innovations
Point-of-care PCR systems are designed to deliver fast, accurate results outside traditional laboratory environments. These compact devices reduce turnaround time and expand testing access in rural or resource-limited areas. By simplifying workflows and integrating automated analysis, they maintain diagnostic accuracy while improving convenience. Such innovations are reshaping decentralized healthcare delivery models.
Conclusion

PCR machines have transformed disease detection by offering unmatched sensitivity, specificity, and speed. From infectious disease surveillance to advanced molecular quantification, PCR remains one of the most trusted diagnostic technologies in modern medicine. As innovation continues, its role will only expand, supporting faster diagnoses, smarter treatment strategies, and stronger global health systems.
Read More Informative Information At Mypasokey